What is PSA?
PSA (prostate-specific antigen) is a small protein molecule which is normally found in seminal fluid (semen) released from the prostate gland during ejaculation. A very small amount is also released into the bloodstream. As you get older, your prostate slowly enlarges and produces more PSA, so your blood level gradually increases. The larger your prostate, the higher the blood test PSA.
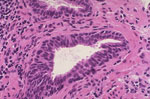 Prostate cancer (pictured right) also becomes commoner with increasing age. By the age of 90 years, almost all men will have microscopic areas of tumour in their prostate. This does not mean that they have active prostate cancer. Many elderly men live a normal lifespan without the need to treat these "incidental" tumours.
Prostate cancer (pictured right) also becomes commoner with increasing age. By the age of 90 years, almost all men will have microscopic areas of tumour in their prostate. This does not mean that they have active prostate cancer. Many elderly men live a normal lifespan without the need to treat these "incidental" tumours.
Other factors that can increase your chances of developing prostate cancer include:
- having a first degree relative (father or brother) with prostate cancer,
- being of Black-African or Black-Caribbean heritage;
- carrying a BRCA gene mutation or:
- being obese.
Only detailed urological investigation can determine whether a prostate cancer is "incidental" (requiring no treatment) or "significant" (requiring active treatment).
What should I do if I have a raised PSA?
If you have a raised PSA or you have been told that your prostate feels abnormal, you should contact your GP or your urologist for further advice
What are the facts about a raised PSA?
The PSA blood test is not a specific test for prostate cancer; raised levels may also be caused by inflammation, infection or benign enlargement of the prostate, ejaculation, vigorous exercise within 48 hours of the test, recent surgery, other procedures to the prostate, urethra or bladder, or problems with urination.
PSA levels can fluctuate so, if your PSA is raised, your doctor may repeat your blood test, to be sure that the value is still above normal limits, before arranging further investigations;
There is no "normal" level of PSA, but there are guidelines that doctors use to identify men at risk of prostate cancer, based on their PSA result.
- with PSA levels between 3 and 10, approximately 25% of men have prostate cancer on biopsy;
- higher levels of PSA make prostate cancer more likely (50% chance with a PSA greater than 10);
What should I expect when I seek further advice?
Your GP will normally assess your general health, and ask about any prostate symptoms you may have. You may have tests of kidney function, bone function, liver function and your GP may check your blood cells for anaemia or other abnormalities.
Your doctor may perform a urine test to exclude infection as a cause of an elevated PSA.
Your doctor may examine your prostate, but this is not essential' declining a prostate examination should not prevent you from having a PSA blood test, or from being referred for further testing.
If your PSA is raised ,or your GP suspects that your prostate feels abnormal, a referral will be arranged for you to see a urologist using the fast-track (2-week wait) system.
What happens next?
In the fast-track urology clinic, you will usually assessed over the telephone by a urologist or a urology nurse specialist. Based on this assessment, you may be advised to have further investigation with an MRI scan of your prostate.
What is multi-parametric magnetic resonance imaging (mp-MRI)?
MRI is a scanning technique that uses strong magnetic fields and radiowaves to produce a detailed image of your prostate. Experienced radiologists can examine these images to measure the size of your prostate and see whether there are any suspicious areas within the prostate that may be cancer.ous
If the MRI scan is clear (reported as low risk), then there is a 90% chance that you do not have a significant prostate cancer. If your prostate is enlarged, or there are other reasons to explain the raised PSA level, you may be reassured that no further investigation is necessary at this time. You are likely to be advised to have further PSA tests in the future, and be given a personalised PSA level, above which, you should be referred for another MRI scan. If there is ongoing concern, you may be offered a repeat blood test, scan or biopsy as a precaution.
If the MRI scan is suspicious for prostate cancer, you may be advised to have a biopsy of your prostate. Any abnormal areas can then be targeted with reference to the MRI scan. Your urologist will discuss your individual situation with you.
If the MRI scan is equivocal (neither low or high risk) and the PSA is high for the size of your prostate, or there are other reasons to suspect prostate cancer, you are likely to be offered a biopsy. If however, your prostate is enlarged, and the PSA is appropriate for the size of your prostate, you may not need a biopsy: instead, you may be be recommended to have further PSA tests in the future, and be given a personalised PSA level, above which you should be referred for another MRI scan.
Download a leaflet about prostate biopsy
What happens once the biopsies have been performed?
 It may take a couple of weeks before you get the final results of your prostate biopsies. The biopsies are analysed under a microscope (pictured right) to determine whether prostate cancer is present. If it is, the tissue is examined in more detail to determine the grade of cancer (the Gleason grade). This is done by looking at the characteristics of individual groups of cancerous cells.
It may take a couple of weeks before you get the final results of your prostate biopsies. The biopsies are analysed under a microscope (pictured right) to determine whether prostate cancer is present. If it is, the tissue is examined in more detail to determine the grade of cancer (the Gleason grade). This is done by looking at the characteristics of individual groups of cancerous cells.
Once the biopsies have been examined carefully, the results will be discussed in a multi-disciplinary team (MDT) meeting where a number of specialists will consider your case in detail.
If your prostate biopsies are negative for prostate cancer, you will normally be advised to have repeat PSA blood tests and, occasionally, a further MRI scan to check any suspicious changes have resolved.
If your prostate biopsies are positive for prostate cancer, your urologist will then discuss the following:
Staging investigations
To find out the extent of your prostate cancer, your urologist may arrange a CT scan, a bone scintigram (bone scan, pictured), or a PSMA PET scan. Together with the PSA level, Gleason grade found on the biopsies, these will determine what treatment is needed. Not all patients, however, require staging investigations before treatment.
Treatment options
Once the results of all the tests are available, your urologist will discuss what treatment options are available and what is best for you. This will take into account your life expectancy, general health, as well as the risk of the cancer (based on PSA level, biopsy features and stage of the tumour)
Based on the factors above, your urologist will help you decide whether the cancer can be safely monitored, or whether treatment would be beneficial. If treatment is required, There are many ways of doing so, including by surgery, radiotherapy, hormonal treatment, chemotherapy or ultrasound (HIFU). If your tumour is at low risk of getting worse, it may be more appropriate for your cancer to be closely monitored (known as active surveillance) and treated only if there are signs of progression.
Information about active surveillance
For some patients, particularly those with a short life expectancy, or other more serious medical conditions, neither immediate treatment or monitoring may be necessary, with treatment only required if the cancer causes symptoms in the future.
Page dated: July 2024 - Due for review: August 2026